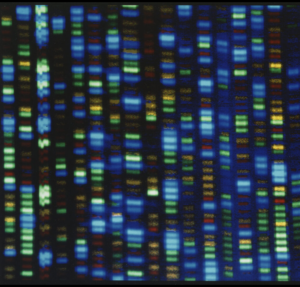
Lurking in colonies of pathogenic bacteria are drug-resistant mutants. If the colony is exposed to antibiotics, these resistant mutants may survive, but they still face the challenge of recolonizing the host. Their success in this task depends on their diversity; a diverse population is more likely to harbor mutants that can withstand a second threat, such as the host’s immune response or another wave of antibiotics. Understanding the factors that contribute to diversity after a population bottleneck can help predict whether bacteria will rebound. Intuitively, it would seem that the more cells that survive, the more diverse the colony will be. Indeed, the number of types of mutants scales with colony population size. But under some conditions, Couce et al. show in the July issue of GENETICS, larger populations may actually be less diverse—and, as a result, more vulnerable to a second blow.
The key is that diversity isn’t defined solely by the number of mutant types: It also depends on how well-represented each type of mutant is in the population. This can be quantified by calculating the probability that two mutants chosen at random from a population will be siblings. Using a mathematical model, the researchers demonstrated that in a resistant subpopulation left standing after an antibiotic-induced bottleneck, diversity is only proportional to population size if the mutant’s growth rate is slower than or equal to the growth rate of the parent clone. If mutants grow faster, they become overrepresented in the population. As the population size increases, the faster-growing mutant clones overtake the rest in number, making the distribution of mutants more and more uneven.
To qualitatively verify their finding, the researchers used simulation and experimentation. Simulations allowed them to take into account factors such as “jackpot” events, in which a population is rich in mutants because of a mutation that appeared near the beginning of the colony’s growth. As would be predicted, “jackpot” events significantly reduced the diversity of resulting populations, but this effect didn’t change the fact that when mutants grow faster than wild-type, diversity is consistently lower.
As an empirical test, the researchers subjected large and small populations of the pathogenic bacteria Pseudomonas aeruginosa to the antibiotic fosfomycin. The researchers selected P. aeruginosa because it’s known that a mutation disabling a single gene is the only way these bacteria can resist fosfomycin, and mutations in this gene do not alter growth rate in the lab. When subjected to sublethal concentrations of fosfomycin, knocking out the resistance gene allows the mutants to grow 2.7 times faster than wild-type bacteria. In agreement with their model, the researchers found without fosfomycin, diversity increased as population size increased, since the mutants grew at the same rate as the wild type. In the presence of sublethal doses of the drug, in contrast, diversity remained low even in very large populations consisting of of several hundred billion individuals.
Since bacteria are routinely subjected to sublethal concentrations of antibiotics, these results may help us better understand how and why bacterial infections rebound as well as the emergence and spread of antibiotic-resistant “super-bugs.” The findings may also aid in the study of antitumor therapy because these treatments involve placing similar stressors on tumor cells. Other researchers have already demonstrated that the genetic diversity of a tumor predicts its response to various treatments, so understanding how and why this occurs could help inform infectious disease and cancer therapies alike.
CITATION:
Couce, A.; Rodríguez-Rojas, A.; Blázquez, J. Determinants of Genetic Diversity of Spontaneous Drug-Resistance in Bacteria.
GENETICS, 203(3), 1369-1380.
DOI: 10.1534/genetics.115.185355
http://www.genetics.org/content/203/3/1369


![This colorized version of PHIL 232 depicts a scanning electron micrograph (SEM) of a number of Pseudomonas aeruginosa bacteria. Photo and caption credit: Janice Haney CarrContent Providers(s): CDC/ Janice Haney Carr [Public domain], via Wikimedia Commons.](https://s43361.pcdn.co/wp-content/uploads/2016/07/rsz_1pseudomonas.jpg)