A strain of Staphylococcus epidermidis isolated from a hotel room may provide insight into how resistance develops outside of medical settings.
Although intense research and media interest has focused on drug-resistant bacteria in hospital settings, resistance can and does evolve outside the clinic. Methicillin-resistant Staphylococcus epidermidis is often isolated from infections of medical devices, but in a report in G3: Genes|Genomes|Genetics, Xu et al. studied drug resistance in a strain that was isolated from a public setting: a hotel room in London.
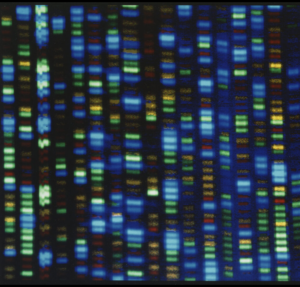
Although S. epidermidis isn’t as virulent as its infamous relative S. aureus, it can still cause infection and serve as an important reservoir for resistance genes, which can be transferred to more deadly bacteria. The authors sequenced the genome of their strain and tested its susceptibility to a panel of antibiotics.
After sequencing the new strain’s genome, the authors found that its chromosome and six plasmids contained a number of resistance genes, including the fosfomycin resistance gene fosB, the multidrug resistance gene msrA, and several others. A comparison between the hotel strain and other sequenced S. epidermidis genomes revealed that some of these genes were unique to the new isolate, such as the tetracycline resistance gene tet(K). They also tested the strain’s susceptibility to a panel of thirteen antibiotics and found that it was resistant to eleven of them.
This is the first genomic analysis of an S. epidermidis strain isolated from a general public setting, and it demonstrates how antibiotic resistance can occur even outside of the specific evolutionary pressures of a sterile healthcare setting. More studies like this may help us to further understand—and combat—the spread of antibiotic-resistance among our ever-present bacterial guests.
CITATION:
Whole Genome Sequence and Comparative Genomics Analysis of Multi-drug Resistant Environmental Staphylococcus epidermidis ST59
, , , , , ,